What is Leaky Gut? Do You Have It & How To Fix It
Leaky Gut Syndrome has been in the media a lot recently. Maybe you’ve been diagnosed with it, or know someone who has? Or maybe you’ve never even heard of Leaky Gut. After reading this article, you will know what Leaky Gut is. And if you have any of the classic symptoms of Leaky Gut, what to do about it.
Leaky Gut has been linked to a wide range of autoimmune diseases including asthma, celiac, IBS, lupus, rheumatoid arthritis, chrons, colitis, diabetes, heart disease, MS, fibromyalgia, migraines, and other headaches. Even anxiety, depression, dementia, and Alzheimer’s have been linked to Leaky Gut. While Leaky Gut Syndrome isn’t a disease itself, it can lead to other diseases that no one wants to get.
Just about anyone diagnosed with an autoimmune disease most likely also has enhanced intestinal permeability or Leaky Gut. It might be a chicken-and-egg thing, did the autoimmune cause the Leaky Gut or vice-versa? Research is pointing the finger at Leaky Gut as the precursor of most autoimmune diseases—not the other way around.(1)
Twenty-plus years ago I was diagnosed with Celiac, long before many people had even heard of it. Leaky Gut (caused by a mega-dose of antibiotics after food poisoning in Thailand) was the trigger for my Celiac. I’ve been dealing with Leaky Gut on and off for the past twenty years. And I have learned a lot about it, as well as many ways to treat it.
So what is a leaky gut?
Let’s start with a little primer on the digestive system, or “gut”. Think of your intestinal tract as one long tube from your mouth to your anus. Kind of like the hole of a donut, it’s actually “outside” your body. Your skin’s job is to help keep toxins out of your body. And your intestinal tract has a similar job of keeping toxins out of your body too. With the exception of nutrients like amino acids, vitamins, and minerals absorbed from digested food—everything else that enters your mouth should stay out of your body. This includes toxins, bacteria, and bits of undigested foods.
Unfortunately, sometimes things go haywire, and toxins, bacteria, and bits of undigested foods make their way inside your body. No bueno!
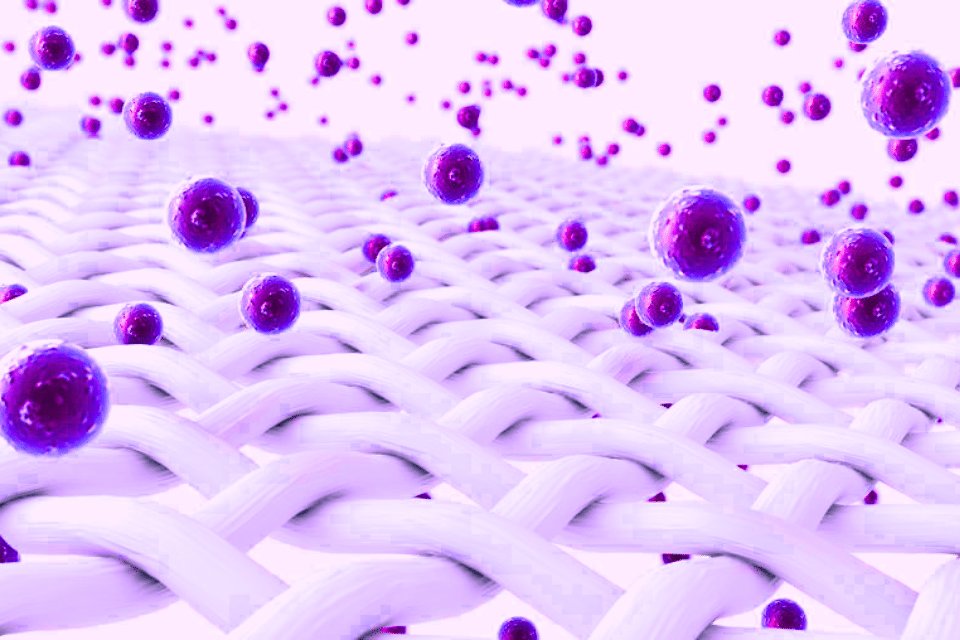
In simple terms, Leaky Gut is a condition where the lining of your intestinal tract gets “holes” in it like a sieve. While that’s an easy way to think of it, it’s not exactly correct. According to Harvard Health, “Inside our bellies, we have an extensive intestinal lining covering more than 4,000 square feet of surface area. When working properly, it forms a tight barrier that controls what gets absorbed into the bloodstream.”(3) But with enhanced intestinal permeability the cells that make up this one-cell thick intestinal wall lining, or “epithelial tissue”, start to pull away from each other, leaving gaps between the cell-walls. These gaps then allow undigested food, bacteria, and other toxins to enter the body, a place where they don’t belong.
What causes enhanced intestinal permeability?
Our gut plays host to over 500 species of microbes that make up our microbiome(4), most are “good” and some are “harmful”. These bacteria help do everything from aiding digestion and providing us with vitamins and nutrients to balancing our immune system and creating 95% of the serotonin (our body’s own “Happiness drug”).(6) So as you can imagine, without the right gut bacteria, our immune systems may crash, along with our sense of happiness and a whole host of other things can start to go wrong.
“Simply put, your gut microbial ecosystem must be healthy for you to be healthy. When your gut bacteria are out of balance — when you have too many pathogenic bacteria and not enough healthy bacteria —you get sick.”(5) —Dr. Mark Hyman, MD
The good bacteria in our gut microbiome are also the “gatekeepers” to the intestinal lining, ensuring that nothing bad gets through. But when the good microbes become depleted, or under attack by too many harmful microbes, they can’t defend the gut lining, and enhanced intestinal permeability (“leaky gut”) starts to occur.
Is your gut a nylon stocking or a fishnet stocking?
Here is a fun analogy you can use to visualize a leaky gut. Think about the tightly woven mesh of a nylon stocking. If you filled it with a smoothie, the liquid would slowly seep out leaving some food particles inside. This is how your intestinal lining is meant to work and get nutrients into your body (slowly seeping in). However, with enhanced intestinal permeability, as the cell walls become damaged or inflamed they pull away from each other. And that tight mesh of the nylon stocking suddenly turns into more of a fishnet stocking.
Now think about what happens when you fill a fishnet stocking with a smoothie. The whole smoothie gets through the fishnet, right? Similarly, in a “leaky gut,” undigested food particles get through the intestinal lining where they don’t belong. Since the majority of your immune system resides on the backside of the intestinal lining—it’s there to react when things like small bits of undigested food get through (think “stranger danger”!)—it creates an immune response and inflammation.
There are many other things that can lead to enhanced intestinal permeability. Here is a list of the major known factors. Some of these factors affect all people, some only affect people with a predisposition to that factor. This is not a complete list as the concept of bio-individuality shows us different factors can affect people differently. But most people with Leaky Gut (enhanced intestinal permeability, or EIP) have reacted to one or more of these factors.
Multiple factors contribute to Leaky Gut
- Alcohol ~ Consuming Alcohol can damage normal functions of the intestinal tract in a couple of ways. Alcohol appears to reduce a substance in the body called prostaglandins which helps control inflammation. In turn, the inflammation can then trigger or exacerbate Leaky Gut syndrome.(7)
- Antibiotics ~ While antibiotics can be very helpful in certain situations, most antibiotics wipe out all the gut bacteria—both good and harmful, leaving your gut with no defense mechanism. Because antibiotics have been seriously overprescribed in the past 50 years, many people now have a compromised gut microbiome. It’s interesting to note that Strep Throat (streptococcal bacteria) will go away entirely on its own within five days, without any antibiotics at all. How many other similar bacteria would also vanish on their own without our taking antibiotics and damaging our gut microbiome in the process?
- Asprin and NSAIDS ~ Painkillers and anti-inflammatories like aspirin and NSAIDs (ibuprofen, Aleve or Naproxin) are known to irritate the intestinal lining and can lead to Leaky Gut with prolonged use.(8)
- Birth Control Pills (BCPs) ~ Many people don’t realize that the sex hormones estrogen and progesterone don’t belong in our guts, and would never, EVER end up there naturally. So the artificial estrogen and progesterone hormones found in oral contraceptives can really wreak havoc on our gut microbiome, causing damage that can last for years after BCPs are stopped. In fact, the use of BCPs is associated with a 50% increased risk of developing Crohn’s disease.(9)
- C-section Birth ~ Interestingly, a baby has a sterile intestinal tract prior to birth, and if it’s born naturally, its gut is populated with the correct microbiome from the mother in the birth canal. However, new research has shown that the gut microbiome of babies who are born via C-section gets populated with skin bacteria instead of normal gut bacteria.(10) Having skin bacteria in the gut can potentially lead to Leaky Gut. And since C-sections are on the rise worldwide, partly due to the “convenience” of scheduling a birth, these babies are more at risk for developing autoimmune diseases.
- Dairy ~ While dairy is the perfect food for baby cows, it turns out that it might not be so great for adult humans. More than 75% of adult humans have a sensitivity to dairy. Most don’t know it or are in denial because they love their dairy so much that they are willing to put up with seemingly minor symptoms to keep eating it. But what people might not realize is that eating dairy and other known allergen foods (like corn, soy, eggs, and nuts) that don’t love them back could be doing major damage to the epithelial lining in their intestines.
- Gluten ~ Research indicates that regardless of Celiac or non-Celiac gluten sensitivity, ingesting gluten can increase gut permeability across the board for everyone. This is partly due to the fact that gluten-containing grains like wheat and barley have been hybridized over the past 50+ years to contain much more gluten. Breads of yesteryear were naturally fermented (like sourdough) and the natural fermentation process broke down and dissolved much of the gluten. Note: this does NOT mean that gluten-sensitive or Celiacs can eat sourdough bread, as it will still contain some gluten, just not as much. And most gluten-containing grains are now sprayed with glyphosate, which binds to the gluten. So the immune system may actually be reacting to the glyphosate as much as the gluten.
- Glyphosate ~ This carcinogen is a major ingredient in Monsanto/Bayer’s herbicide Round-Up. The WHO has named it a known carcinogen, and it is being banned in many countries around the world (including France, Netherlands, Belgium, and Germany—but not the US yet.) It’s also thought to be one of the top killers of our own gut microbiome. It has been shown to have deleterious effects on insects in addition to plants. And since our microbiome “bugs” are biologically very similar to insects, it can wipe them out too. It’s also now sprayed on most grains prior to harvesting, as a desiccant to make them easier to harvest. Glyphosate levels in humans have been on the increase in the past few years. (11)(12)
- Lack of Exercise ~ Research is now shedding light on how exercise supports your gut microbiome.(13) Besides all of the other health benefits of a regular exercise program or staying active and moving your body every day, it appears that exercise enhances your good gut bacteria, helping them support your intestinal lining.
- Lack of Sleep ~ Sleep is vitally important to many systems in your body, including maintaining a healthy gut microbiome. Interrupting your circadian clock in the form of poor quality sleep, lack of sleep, working graveyard shift, and/or late-night eating has been shown to have harmful effects on your gut microbes.(14)
- Low-fiber Diets ~ The digestion system needs fiber to stay healthy. Sadly, the Standard American Diet (SAD) tends to be low-fiber, so many people are missing out on needed fiber. But fiber-containing foods are actually “pre-biotics” that feed the good gut bacteria and keep them happy. Foods high in prebiotics include: lentils, chickpeas, beans, oats, bananas, Jerusalem artichokes, jicama, asparagus, garlic, leeks, onions, and nuts.
- Smoking Cigarettes ~ Just one more reason to quit smoking if you still do. The thousands of toxins in cigarettes (70 of which also cause cancer) do a number on your good gut bacteria, wiping out most of them.(15)
- Stress ~ Stress, both long-term and short but acute periods of stress, can also contribute to Leaky Gut. Studies show stress can have both short- and long-term effects on the functions of the gastrointestinal tract.(16) And most of us could probably do a lot to mitigate our stress levels.
- Sugar ~ As more and more light is shed on the health risks of eating sugar, Leaky Gut is another one. Sugar is highly inflammatory and can cause an overgrowth of harmful gut bacteria, over-running the good gut bacteria, wiping out the guards to the gut lining, as well as inflaming the epithelial cells.
What are the symptoms of leaky gut?
Now that you know some of the things that can lead to Leaky Gut, do any resonate with you? If so, here are some of the symptoms of enhanced intestinal permeability that you need to look out for.
“Some people may have a weaker barrier because they were born with it, or they follow an unbalanced diet low in fiber and high in sugar and saturated fats, which may be the trigger that weakens the gut lining. Age also plays a role because as you age, cells get damaged more easily and heal slowly, if at all, so the gut becomes more vulnerable.”
—Harvard Health,
The gut and brain are directly linked and communicate via the vagus nerve. So a dysfunctional gut can directly affect the brain. This is one of the reasons that people with Leaky Gut can experience a wide array of symptoms, ranging from physical to mental and emotional. And this wide range of symptoms can also make Leaky Gut hard to diagnose. This has also led many MDs to not believe that Leaky Gut exists. However, in recent years, there have been many studies on Leaky Gut. And there are now over 16,000 published studies on Enhanced Intestinal Permeability on PubMed.gov. So it is definitely acknowledged by research today, even if not by your doctor.
The following are some but not all of the symptoms experienced by people with leaky gut:
- Arthritis and joint pain
- Brain fog, headaches, dementia, Alzheimer’s
- Chronic diarrhea, constipation, gas, bloating, or stabbing stomach pains
- Depression, anxiety, ADD, ADHD
- Fatigue
- Nutritional Deficiencies
- Skin rashes, acne, eczema or rosacea
- Whole food particles in stools
So can you repair enhanced intestinal permeability?
All these symptoms can seem overwhelming, and the thought of them leading to autoimmune diseases even more so, right? But the good news is that Leaky Gut can be repaired fairly quickly with the right dietary and lifestyle modifications.
One of the first steps to repairing Leaky Gut is to do an elimination diet to rule out any known foods that might be causing an issue. This is one of my areas of expertise, working with clients to rule out food sensitivities or intolerances, and helping to heal their Leaky Gut.
Once the triggering foods have been determined, they must be eliminated at least until the gut lining and microbiome have been repaired. This may be a matter of weeks to months, depending on the individual, the severity of the damage, and how long it’s been going on.
The epithelial lining is one of the fastest regenerative cells in the body. It can actually regenerate every 5 to 7 days, provided that the gut microbiome is supporting it and doesn’t continue to inflame it as it is trying to repair itself.
How to help your gut heal
That’s not to say that your Leaky Gut will be cured in 5 to 7 days. That is just the beginning of repairing the epithelial lining as well as the gut microbiome to support a healthy gut in the future. You need to ensure you’re not eating any of the foods that aggravate it. And you’ll likely need to take some digestive enzyme supplements and probiotics to help with the repair as well.
In severe cases, a fecal transplant may be warranted. This would be something to discuss with an MD when all else fails.
Besides eliminating the known foods and above-mentioned habits that are known to contribute to Leaky Gut, eating foods and supplements like bone broth, organic apple pectin, aloe vera gel, slippery elm, and marshmallow root, will all help to support repair of the gut lining.
Why many MDs don’t believe leaky gut exists
“When I was at the Mayo Clinic training with the Internal Medicine Service, we would see patients with chronic autoimmune disease…And I would whisper because it was not accepted as a real clinical term in medicine, “Do you have leaky gut?” At this point, the attending physician, who was my mentor, would stop me and ask how could this have anything to do with the patient’s problem. And exactly what kind of alternative medicine was I trying to practice?”
— Dr. Mark Menolascino, M.D.
Sadly, many doctors still don’t believe Leaky Gut exists or deny that it can lead to autoimmune diseases. It’s not entirely the doctor’s fault. It is partially due to the fact that many med schools are backed by big pharma, and doctors are taught “a pill for every ill”.
Looking at the list of causes above, you can see that most of them are either foods that could be eliminated from or added to the diet or habits that can be reversed like smoking cessation, improved sleep, more exercise, and meditation for stress. You don’t need a “pill” to reverse a Leaky Gut. In fact, many medications contribute to or exacerbate the problem. Since there isn’t much money to be made in “curing” Leaky Gut, big pharma doesn’t endorse it. And med schools don’t teach it.
Thankfully that’s changing with the development of Functional Medicine. And many forward-thinking MDs like Dr. Mark Hyman, Dr. Terry Wahls, Dr. Sarah Gottfried, Dr. Amy Myers, and Dr. Mark Menolascino(2) are leading the way in progressive and Functional medicine, with thousands of case histories to back up the evidence that Leaky Gut is a “thing”, that it does lead to autoimmune diseases, and that for the most part, it’s also fairly easily treatable.
What to do if you suspect leaky gut?
As a Certified Holistic Health & Nutrition Coach, I work with clients to determine which foods and habits may be contributing to or exacerbating Leaky Gut symptoms. Then we make a plan to resolve them and rebuild the gut lining. If you suspect you have a Leaky Gut, schedule a call, I’d love to help!
Please share this article with others who may benefit from it, and leave a comment to let us know your experience dealing with Leaky Gut, or your biggest takeaway from this article.
—————————-
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440529
- https://menoclinic.com/dr-marks-integrative-medicine-cabinet-pharmacy-kitchen
- https://www.health.harvard.edu/blog/leaky-gut-what-is-it-and-what-does-it-mean-for-you-2017092212451
- https://drhyman.com/blog/2018/04/13/how-to-feed-your-gut
- https://drhyman.com/blog/2015/08/26/10-strategies-to-eliminate-ibs-and-create-good-gut-health
- https://www.apa.org/monitor/2012/09/gut-feeling
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2614138/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4425136
- https://pubmed.ncbi.nlm.nih.gov/18684177/
- https://www.nature.com/articles/s41467-018-07631-x
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5515989
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6322310
- https://www.ncbi.nlm.nih.gov/pubmed/25825908
- https://www.ncbi.nlm.nih.gov/pubmed/21673361
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3597605
- https://www.ncbi.nlm.nih.gov/pubmed/22314561
